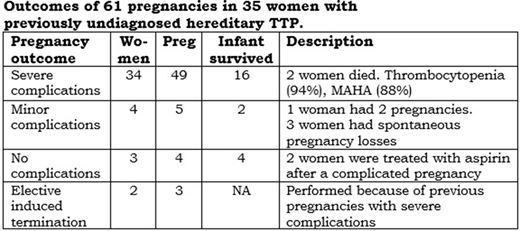
Critical complications of pregnancy in women with hereditary thrombotic thrombocytopenic purpura (TTP) have been recognized since hereditary TTP was first described and they continue to be frequently reported. However, the frequency of complications, their severity, and when they occur during pregnancy are not known. We reviewed all case reports of patients with hereditary TTP whose diagnosis was confirmed by documentation of ADAMTS13 activity <10% and biallelic ADAMTS13 mutations. We identified 80 articles (180 patients) by searching MEDLINE and PubMed from 2001-March, 2020. 44 women were pregnant preceding their diagnosis of hereditary TTP; 9 had insufficient data for analysis. The remaining 35 women had 61 pregnancies (2 with twins). Major complications were defined as life-threatening, requiring urgent hospitalization. Other complications were defined as minor. 34 (97%) women had severe complications during one or more pregnancies (Table). 31 women had severe complications with their first pregnancy; 3 had spontaneous pregnancy losses at 5-11 weeks' gestation and then severe complications with their second pregnancy. Of the 31 women who had severe complications during their first pregnancy, 21 had no report of a subsequent pregnancy. 49 (84%) of the 58 pregnancies (excluding 3 pregnancies with elective induced termination) had severe complications. Gestational age was reported for 41 (84%) of the 49 pregnancies with severe complications; they occurred from 7 to 37 weeks' gestation (median, 23 weeks). 12 (29%) occurred at <20 weeks' gestation, when preeclampsia rarely occurs; 7 (17%) occurred in the first trimester. Among the 49 pregnancies with severe complications, outcome was reported for 48 infants; 16 (33%) survived. In 22 patients, pregnancy complications may have been the initial symptoms of hereditary TTP. Only 3 women had uncomplicated pregnancies, each following an initial pregnancy with severe complications; 2 women (2 pregnancies) were treated with aspirin throughout their pregnancy. 2 (6%) of the 34 women died from severe complications of their initial pregnancy. The risk of death with pregnancy may be greater than 6% because in 4 of the 29 families, an older sister had died from pregnancy complications but TTP was not suspected, ADAMTS13 activity was not measured. If these 4 women had been documented to have hereditary TTP, the frequency of deaths during pregnancy would have been 17%. The severe complications had the typical clinical features of TTP: thrombocytopenia, microangiopathic hemolytic anemia (MAHA); their symptoms were similar to features of severe preeclampsia. The diagnosis of TTP should be considered and ADAMTS13 activity measured in all women who have unusually severe or atypical preeclampsia. When TTP is diagnosed during pregnancy, both hereditary and acquired TTP should be considered. When hereditary TTP is diagnosed, plasma prophylaxis is required for all subsequent pregnancies. We begin plasma prophylaxis as soon as pregnancy is documented, adjusting the amount and interval to maintain the patient's normal platelet count; we continue plasma prophylaxis for 6 weeks postpartum. Prophylactic plasma can prevent exacerbations of TTP but it does not prevent the occurrence of preeclampsia.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal